Document Type : Review Article
Authors
1 Associate Professor of Cardiac Anesthesia, Department of Anesthesiology, School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
2 Assistant Professor of Obstetrics and Gynecology, Department of Obstetrics and Gynecology, School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Introduction: considering that intravenous acetaminophen is currently usually injected as a bolus, in such a way that it should be injected for 20 minutes and 4 times a day to patients undergoing surgery, and considering the lack of nurses and the fact that practically This work is not cost-effective in terms of time and money, and there was no research in the field of intravenous drip injection within 24 hours. Therefore, this study was conducted with the aim of investigating the effectiveness of intravenous acetaminophen injection during the first 24 hours after cesarean section in a systematic review.
Methodology: In this review article, all databases including Google Scholar, Scopus, Web of Science, PubMed, SID, MagIran, and the Cochrane Library were searched and reviewed by both authors of this article based on PRIZMA guidelines without time and language limitations. The keywords included Pain, Pain relief, Postoperative Pain, Pain Decrease, Cesarean Section, Acetaminophen, and Paracetamol.
Results: Ten studies were included in this study. Examining the results indicated that intravenous injection of paracetamol leads to a decrease in pain intensity during the first 24 hours after elective cesarean section.
Conclusion: Intravenous injection of acetaminophen for pain control after cesarean section by PCA pump, in addition to proper pain control, maintains the hemodynamic indicators of patients well and does not have an adverse effect on the time of walking after the operation.
Graphical Abstract
Keywords
Main Subjects
Introduction
Abdominal surgery is a painful process, which control the pain and the complications caused by it causes the early discharge of these patients. Therefore, in these cases, pain relief after surgery is very important [1-3]. For this reason, improving pain control methods after surgery has become very important for anesthesiologists [4-6].
Today, anesthesiologists have taken a very effective step in this field by inventing Patient Control Analgesia methods. Various methods are used for pain relief in these patients, which can generally be classified into the following four categories: systemic narcotic analgesics, systemic non-narcotic analgesics, intrathecal narcotics, and epidural narcotics [7-9].
The usual method of post-operative pain relief is the use of narcotics. Because of the increased incidence of nausea and vomiting and the possibility of respiratory complications, they are injected with the lowest dose [10-13]. Today, intravenous acetaminophen under the brand name of Apotel is one of the common drugs in operating rooms and inpatient wards to control the pain of patients [14-16].
This drug belongs to the category of pain reliever, anti-fever medicine, and its pharmaceutical form is an injection ampoule containing one gram of paracetamol in 6.7 ml (Figure 1). This drug exerts its effects with the following three mechanisms:
- Preventing the secretion of prostaglandins in the CNS,
- Reducing environmental anti-inflammatory effects, and
- Reducing fever with a direct effect on the temperature control center in the hypothalamus.

Figure1. Paracetamol molecule
Acetaminophen has analgesic and antipyretic effects similar to aspirin, but its site of action and its analgesic mechanism are not well understood [17-19]. This drug exerts its analgesic effects by inhibiting central cyclooxygenase 1 and 2, and probably by directly affecting the serotonergic system [20]. The phenomenon of nurses leaving the service has become the concern of many countries [21].
In recent years, the issue of the shortage of nurses in Iran has become a concern for managers and a fundamental challenge for the health care system. According to the definition, attrition is a process in which employees leave the organization or are transferred to the other departments or units of the organization.
Of course, this definition does not specify the voluntary or involuntary nature of leaving the service of members [21-23]. On the other hand, nurses are a vital part of the health care system, so that as the largest group, they constitute about 56% of hospital employees [24].
According to the above explanations, it seems necessary and necessary to make plans to reduce nursing duties by considering the best results for patients. Today, to relieve pain after surgery, Apotel is used abundantly and in the form of multiple injections during one day and night, which causes excessive spending of time, money, and nursing services. If it is determined that the administration of intravenous acetaminophen in the form of a 24-hour drip has a suitable analgesic effect with fewer complications for patients after caesarean section, it can be used as a more suitable instruction for intravenous acetaminophen administration. Caesarean section surgery is one of the most common surgical procedures for women, and pain after surgery is one of the most important problems among this category of women [28-30]. The results of recent research have shown that intravenous acetaminophen is useful and effective for relieving the pain of these women after cesarean surgery [31-33].
Using the combination of different drugs with the PCA pump can, in addition to reduce the amount of narcotics used, reduce drug side effects, and increase satisfaction in patients and treatment staff [34-36].
Due to the fact that intravenous acetaminophen is currently usually injected as a bolus, in such a way that it should be injected for 20 minutes and 4 times a day to patients undergoing surgery, and due to the lack of nurses and the fact that this in terms of time and cost, it is not cost-effective, and there was no such research in the field of intravenous drip injection within 24 hours [37].
We decided to compare two methods of intravenous drip injection and bolus acetaminophen in reducing pain after cesarean surgery. Therefore, this study was conducted with the aim of investigating the effectiveness of intravenous acetaminophen injection during the first 24 hours after cesarean section in a systematic review.
Methodology
In this review article, all databases including Google Scholar, Scopus, Web of Science, PubMed, SID, MagIran, and the Cochrane Library were searched and reviewed by both authors of this article based on PRIZMA guidelines without time and language limitations. The keywords that were selected based on MeSh and searched based on them included Pain, Pain relief, Postoperative Pain, Pain Decrease, Cesarean Section, Acetaminophen, and Paracetamol. These keywords were determined by both researchers in one meeting, and then the search was performed in the mentioned databases by each researcher separately. The search process is given as follow:
Table1. Search strategy in PubMed database based on MeSh criteria
|
(Pain [mh] OR Pain relief [tiab] OR Postoperative Pain [tiab] OR P-perative Pain [tiab] OR Pain Decrease OR Pain Control [tiab]) AND (Cesarean Section [mh] OR C/Section [mh] OR Cesarean/S [tiab] CS[tiab] OR Delivery [tiab] OR Elective Cesarean Section [tiab] OR Elective C/Section [tiab] OR Elective Cesarean/S [tiab] OR Elective C/S[tiab] OR C/S surgery AND Acetaminophen [tiab] OR Paracetamol [tiab] OR Disprol [tiab] OR Hedex [tiab] OR Medinol [tiab] OR Panadol [tiab]) |
The inclusion criteria of studies in this present study included the following:
- The time limit was not applied.
- Language restriction was not applied.
- The studies had clear results.
- The studies had a prospective approach.
- The studies were in the form of clinical trials.
- Randomization was done for all studies.
- The study should be single-blind or double-blind.
- The results of the study are expressed without bias.
- Studies should be of good and high quality.
The criteria for excluding studies from the present study included the following:
- Case studies, reviews, reports of rare cases, letters to the editor, and descriptive.
- The age of the participants should be less than 18 years old.
- The method of randomization is not clearly stated.
- The dosage of the used drugs is not stated.
- There is no control group in the study.
- The expected results have not been achieved.
- Exclusion criteria have not been stated.
- The method of intervention is not clearly stated.
- The conclusion is ambiguous.
After that, the title and purpose of the study were reviewed and evaluated, and studies were included in the review that had a clear purpose in the title and were in line with our study.
Finally, the full text of each article was reviewed by both authors, and the studies that had the appropriate and desirable quality were included in this systematic review.
All the important information of each article was written and recorded separately by both authors in a paper sheet, and then in a face-to-face meeting, the important information was discussed and finally the important information of each article.
Results
A total of ten studies were included in this study. Examining the results indicated that the intravenous injection of paracetamol leads to a reduction in pain intensity during the first 24 hours after elective cesarean surgery (Figure 2).
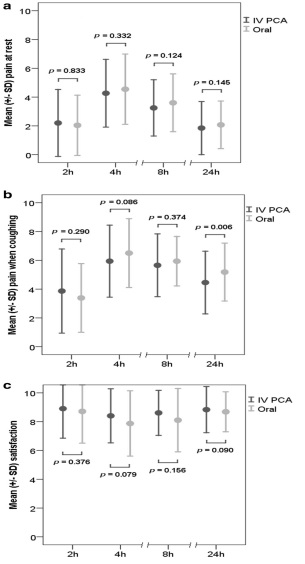
Figure 2. The results of the comparison of pain control status at different hours
The review of the status of the articles also indicated that the publication bias for the studies included in this article is low and the results of this study can be cited (Figure 3).

Figure3. Publication bias chart of studies included in this study
Discussion
Today, pain is considered as the fifth vital sign due to its importance and the need to control it in preventing mortality and complications after surgery. This study was designed and carried out entitled: "Comparison of the effect of intravenous acetaminophen as a 24-hour drip and routine on pain control in patients undergoing cesarean surgery" [44-46].
Female candidates for caesarean section with an average age of 25.81 ± 3.12 years old completed the study. The most common pregnancy ranks were "the first and the second pregnancy". 804 women studied in two groups of 402 were subjected to different pain relief treatment after cesarean section with intravenous acetaminophen.
The importance of pain relief after surgery due to complications such as myocardial ischemia, atelectasis, hypoxia, inability to breathe deeply and cough, decreased respiratory volumes, urinary retention, increased coagulability and thrombosis, immune system suppression, anxiety, insomnia progress towards central sensitization, and chronic pain.
Prescribing non-narcotic analgesics is an essential component of multimodal pain management treatment plans. In this study, the analgesic effect of intravenous acetaminophen administration as a 24-hour drip and routine has been investigated and compared. The present study showed that there is no significant difference between the pain intensity after cesarean in different age groups of women [57-60].
According to the results of the present study, it was revealed that women who were prescribed intravenous acetaminophen on a routine basis had a significant decrease in their average pain intensity during the investigated times after cesarean section. These results show that intravenous acetaminophen is effective in reducing pain after cesarean section.
The researchers showed that injecting acetaminophen before surgery is associated with a reduction in pain after surgery. These results are consistent with the results of our study. On the other hand, the researchers showed that the use of intravenous acetaminophen leads to significant control of pain after cesarean section, and these results are consistent with the results of the present study.
The exact mechanism of action of paracetamol has not been determined, but its effects are probably exerted by inhibiting cyclooxygenase 2 in the brain along with reducing the activity of the serotonergic pathway. It is also effective on the peripheral pain pathways in addition to the central effect.
According to the results of the recent studies, it has been found that paracetamol reduces the periodic contractions that lead to pain, and in this way, it causes proper pain control after cesarean section and reduces the need for narcotic drugs. According to the results of our study, it was shown that women who were prescribed intravenous acetaminophen in the form of a 24-hour drip had a significant decrease in their average pain intensity during the investigated times after cesarean section.
These results indicate the effectiveness of intravenous acetaminophen in the form of a 24-hour drip to reduce pain after cesarean section. Some other researchers showed that intravenous paracetamol has a significant analgesic effect on pain after cesarean section.
Some researchers demonstrated that the administration of intravenous acetaminophen at the end of hysterectomy is effective in controlling pain after abdominal hysterectomy. As can be seen from the above results, the effect of intravenous acetaminophen in the form of a 24-hour drip in reducing pain after cesarean section is greater than intravenous acetaminophen in the form of routine so that the average pain in the 24-hour intravenous acetaminophen drip group is lower than the routine intravenous acetaminophen group.
In a study, researchers reported that intravenous acetaminophen (Apotel) is effective in reducing pain after abdominoplasty. Therefore, it can be a suitable and accessible alternative to opioids in pain relief after surgery. These results are consistent with the results of our study.
Our study showed that there is no statistically significant difference between the walking duration after cesarean section in the two groups of routine intravenous acetaminophen and 24-hour drip. In other words, administering acetaminophen as a 24-hour drip has no effect on the walking duration after cesarean surgery.
Likewise, there was no statistically significant difference between the average heart rate changes in two groups of routine intravenous acetaminophen and 24-hour drip. In other words, administering acetaminophen as a 24-hour drip has no effect on heart rate changes after cesarean surgery. The present study showed that there is no statistically significant difference between the average systolic blood pressure in two groups of routine intravenous acetaminophen and 24-hour drip. In other words, administration of acetaminophen as a 24-hour drip has no effect on the average systolic blood pressure after cesarean section.
While it was shown that the average diastolic blood pressure in the routine intravenous acetaminophen group is significantly higher than the 24-hour drip group. These results show the better effect of administering acetaminophen as a 24-hour drip on the diastolic blood pressure of cesarean section patients.
The results of our study showed that administration of intravenous acetaminophen as a 24-hour drip causes less side effects than routine intravenous acetaminophen in the patient (such as headache, nausea, and vomiting).
These results show that administering acetaminophen as a 24-hour drip can further reduce the pain intensity after cesarean section and reduce side effects in patients. The results of the present study showed that in the group of intravenous acetaminophen in the form of a 24-hour drip, the consumption of diclofenac suppositories was slightly higher than in the group of intravenous acetaminophen in the form of routine.
In a study, researchers showed that the combination of diclofenac suppositories and intravenous acetaminophen can effectively reduce pain after cesarean section. It seems that in future studies, the combined effect of 24-hour intravenous acetaminophen drip with other non-narcotic painkillers can be investigated.
Several studies have been conducted on the role of painkiller pumps on the proper control of post-operative pain with different drug combinations, which show the role of adjuvant drugs to narcotics to reduce the amount of used narcotics and of course reduce the drug side effects and optimize pain control. Patients and improving the performance of nursing care have been taken into consideration, such as the article done in 2019 regarding the use of an analgesic pump in improving pain control after lumbar spine surgery and increasing the satisfaction of patients and the nursing team.
The results of our research showed that the use of acetaminophen drip with an analgesic pump in addition to the background narcotic, in addition to reduce the amount of narcotic used and the complications caused by it, will lead to proper pain control and improve the satisfaction of patients and the nursing team.
According to the review of previous studies, it is necessary to have proper guidelines for pain control in the cesarean section. It seems that an acceptable guideline should be able to reduce the visual score of pain, especially in the first 24 hours, so that effective communication between mother and baby can be established during this time interval.
Likewise, this instruction should minimize the need for drugs. On the other hand, the selected drug should have the least possible side effects and be prescribed in doses lower than the maximum safe dose. Taking paracetamol at intervals and with the right dose can reduce the need for narcotics, and it is better to avoid narcotics as much as possible if the above painkillers are present.
According to this study and similar studies, concerning that taking intravenous acetaminophen as a 24-hour drip causes adequate and appropriate pain control after cesarean section, it seems that using this method is more suitable for prescribing this drug.
Conclusion
The use of acetaminophen drip to control pain after cesarean section by PCA pump, in addition to proper pain control, maintains the hemodynamic indicators of patients well and does not have an adverse effect on the time of walking after the operation.
In addition, its ease of use, besides improving the quality of post-operative care, reduces the pressure on the treatment staff and consequently increases the quality of nursing services. On the other hand, the amount of adverse complications after the operation is reduced compared to routine pain control methods, which in general introduces the use of PCA acetaminophen pump as an excellent method with the least risk for controlling pain after cesarean section.
Conflict of interest
The authors declare that they have no conflict of interest
Consent for publications
All authors agree to have read the manuscript and authorize the publication of the final version of the manuscript
Availability of data and material
Data are available on request from the authors
Funding
Not applicable.
ORCID
Bahman Naghipour
https://orcid.org/0000-0001-5089-1698
Vahideh Rahmani
https://orcid.org/0000-0001-5966-8767
How to cite this article:
Bahman Naghipour* , Vahideh Rahmani. Efficacy of Intravenous Acetaminophen During the First 24 Hours after Caesarean Section: a Systematic Review. International Journal of Advanced Biological and Biomedical Research 2023 11(2) 104-114. Link: http://www.ijabbr.com/article_704903.html
Copyright © 2023 by authors and SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cite
OPEN ACCESS
©2023 The author(s). This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit: http://creativecommons.org/licenses/by/4.0/
PUBLISHER NOTE
Sami Publishing Company remains neutral concerning jurisdictional claims in published maps and institutional affiliations.
CURRENT PUBLISHER
- Haghdoost S M, Gol M K. (2020). The necessity of paying more attention to the neurological and psychological problems caused by the COVID-19 pandemic during pregnancy. Health, 3(4). [Crossref], [Google Scholar], [Publisher]
- Purabdollah M, Tabrizi F M, Khorami Markani A, Poornaki L S. (2021). Intercultural sensitivity, intercultural competence and their relationship with perceived stress among nurses: evidence from Iran. Mental Health, Religion & Culture, 24(7): 687-697.[Crossref], [Google Scholar], [Publisher]
- Aghamohamadi D, Gol M K. (2020). Checklist for determining severity of pain and type and dosage of analgesics administered to patients undergoing breast surgeries. Int J Womens Health Reprod Sci, 8(2): 227-31. [Crossref], [Google Scholar], [Publisher]
- Khanbabaei Gol, Mobaraki-Asl M, Ghavami N, Zharfi Z, Mehdinavaz Aghdam, M A. (2019). Sexual violence against mastectomy women improved from breast cancer. The Iranian Journal of Obstetrics, Gynecology and Infertility, 22(5): 52-60.[Crossref], [Google Scholar], [Publisher]
- Abdollahi M H, Foruzan-Nia K, Behjati M, Bagheri B, Khanbabayi-Gol M, Dareshiri S, Pishgahi A, Zarezadeh R, Lotfi-Naghsh N, Lotfi-Naghsh A, Naghavi-Behzad M. (2014). The effect of preoperative intravenous paracetamol administration on postoperative fever in pediatrics cardiac surgery. Nigerian medical journal: journal of the Nigeria Medical Association, 55(5): 379. [Crossref], [Google Scholar], [Publisher]
- Nazari B, Amani L, Ghaderi L, Khanbabayi Gol M. (2020). Effects of probiotics on prevalence of ventilator-associated pneumonia in multitrauma patients hospitalized in neurosurgical intensive care unit: a randomized clinical trial. Trauma Monthly, 25(6): 262-268. [Crossref], [Google Scholar], [Publisher]
- Nazari B, Amani L, Ghaderi L, Khanbabayi Gol (2020). Effects of probiotics on prevalence of ventilator-associated pneumonia in multitrauma patients hospitalized in neurosurgical intensive care unit: a randomized clinical trial. Trauma Monthly 25(6): 262-268. [Crossref] [Google Scholar] [Publisher]
- Eghdam-Zamiri R, Khanbabayi Gol M. (2020). Effects of ginger capsule on treatment of nausea and vomiting in patients receiving cisplatin undergoing mastectomy: a randomized clinical trial. The Iranian Journal of Obstetrics, Gynecology and Infertility, 22(11): 15-21. [Crossref] [Google Scholar] [Publisher]
- Pourfathi H, Atashkhoei S, Naghipour B, Amini R H, Kafshdooz L. ( 2022). The Effect of Intraoperative Oxytocin Infusion on Irrigation Fluid Absorption During Hysteroscopic Myomectomy: A Randomized Placebo-Controlled Double-Blind Trial. 4(6): 557-566. [Google Scholar] [Publisher]
- Rezaeia S, Naghipourb, Rezaeic B, Dadashzadehd M, Sadeghie M S, Chemical evaluation of gastrointestinal, coronary and pulmonary complications in patients admitted to the intensive care unit. [Google Scholar] [Publisher]
- Naghipour B, Bagerpour M, Shadvar K, Golzari S E, Faridaalaee G. (2022). Effect of hyperglycemia treatment on complications rate after pediatric cardiac surgery. Journal of Cardiovascular and Thoracic Research, 14(1): 18-22. [Crossref] [Google Scholar] [Publisher]
- Sayyah-Melli M, Kazemi-Shishavan M, Behravan N, Mostafa P, Gharabaghi VR. Evacuating Uterine Contents before Operative Hysteroscopy in Patients With Active Uterine Bleeding: A Randomized Clinical Trial. [Crossref] [Google Scholar] [Publisher]
- Sayyah-Melli M, Mobasseri M, Gharabaghi PM, Ouladsahebmadarek E, Rahmani V. (2017). Comparing the effect of aromatase inhibitor (letrozole)+ cabergoline (Dostinex) and letrozole alone on uterine myoma regression, a randomized clinical trial. European Journal of Obstetrics & Gynecology and Reproductive Biology. 210:257-64. [Crossref] [Google Scholar] [Publisher]
- Sayyah-Melli M, Bidadi S, Taghavi S, Ouladsahebmadarek E, Jafari-Shobeiri M, Ghojazadeh M, Rahmani V. (2016) . Comparative study of vaginal danazol vs diphereline (a synthetic GnRH agonist) in the control of bleeding during hysteroscopic myomectomy in women with abnormal uterine bleeding: a randomized controlled clinical trial. European Journal of Obstetrics & Gynecology and Reproductive Biology. 196: 48-51. [Crossref] [Google Scholar] [Publisher]
- Nurmeksela A, Mikkonen S, Kinnunen J, Kvist T. (2020). Relationships between nursing management, nurses’ job satisfaction, patient satisfaction, and medication errors at the unit Level: A correlational study. Research Square. 1(1): 1-22. [Google Scholar]
- Ghahroudi A A, Rokn A R, Shamshiri A R, Samiei N. (2020). Does timing of implant placement affect esthetic results in single‐tooth implants? A cohort evaluation based on mPES. Journal of Esthetic and Restorative Dentistry. 32(7): 715-25. [Crossref] [Google Scholar] [Publisher]
- Hosseini-Khalili AR, Thompson J, Kehoe A, Hopkinson NS, Khoshbaten A, Soroush MR, Humphries SE, Montgomery H, Ghanei M. (2008).Angiotensin-converting enzyme genotype and late respiratory complications of mustard gas exposure. BMC Pulmonary Medicine. 8(1): 1-5. [Google Scholar]
- Birman D. Investigation of the Effects of Covid-19 on Different Organs of the Body. (2023). Eurasian Journal of Chemical, Medicinal and Petroleum Research. 2(1): 24-36. [Crossref] [Google Scholar] [Publisher]
- Karimzadeh F, Sajedi SM, Taram S, Karimzadeh F. (2021). Comparative evaluation of bacterial colonization on removable dental prostheses in patients with COVID-19: A clinical study. The Journal of Prosthetic Dentistry. [Crossref] [Google Scholar] [Publisher]
- Najafi F, Kermansaravi F, Gangoozehi E. The relationship between general health and quality of work life of nurses working in Zahedan teaching hospitals. Iranian Journal of Rehabilitation Research in Nursing. 2018 Feb 10: 4(2):53-9. [Crossref] [Google Scholar] [Publisher]
- Kalantari H, Tabrizi AH, Foroohi F. (2020). Determination of COVID-19 prevalence with regards to age range of patients referring to the hospitals located in western Tehran, Iran. Gene reports. 21, 100910. [Crossref] [Google Scholar] [Publisher]
- Alijanzadeh M. (2015). The frequency of medication errors and factors influencing the lack of reporting medication errors in nursing at teaching hospital of Qazvin University of Medical Sciences, 2012. Journal of Health. [Google Scholar] [Publisher]
- Barzideh M, Choobineh A, Tabatabaei SH. (2012). Job stress dimensions and their relationship to general health status in nurses. Occupational Medicine Quarterly Journal. 4(3): 17-27. [Google Scholar] [Publisher]
- Mileski M, Pannu U, Payne B, Sterling E, McClay R. (2020). The impact of nurse practitioners on hospitalizations and discharges from long-term nursing facilities: a systematic review. InHealthcare 8: 114. MDPI. [Crossref] [Google Scholar] [Publisher]
- Gadlage MJ, Sparks JS, Beachboard DC, Cox RG, Doyle JD, Stobart CC, Denison MR. (2010). Murine hepatitis virus nonstructural protein 4 regulates virus-induced membrane modifications and replication complex function. Journal of virology. 84(1): 280-90. [Crossref] [Google Scholar] [Publisher]
- Asadi N, Salmani F, Pourkhajooyi S, Mahdavifar M, Royani Z, Salmani M. (2020). Investigating the relationship between corona anxiety and nursing care behaviors working in corona's referral hospitals. Iranian Journal of Psychiatry and Clinical Psychology. 26(3): 306-19. [Crossref] [Google Scholar] [Publisher]
- Musaei S. The Effect of Pregnancy on the Skin. (2022). Eurasian Journal of Chemical, Medicinal and Petroleum Research. 2(1): 17-23. [Crossref] [Google Scholar] [Publisher]
- Salehi SH, As’ adi K, Mousavi SJ, Shoar S. (2015). Evaluation of amniotic membrane effectiveness in skin graft donor site dressing in burn patients. Indian Journal of Surgery. 77: 427-31. [Crossref] [Google Scholar] [Publisher]
- Salehi SH, Fatemi MJ, Aśadi K, Shoar S, Der Ghazarian A, Samimi R. (2014). Electrical injury in construction workers: a special focus on injury with electrical power. Burns. 40(2): 300-4. [Crossref] [Google Scholar] [Publisher]
- Nazardani SZ, Nourizadeh Dehkordi S, Ghorbani A. (2022). A comprehensive evaluation of the Sports Physiotherapy curriculum. Eurasian Journal of Chemical, Medicinal and Petroleum Research. 2(1): 10-6. [Crossref] [Google Scholar] [Publisher]
- Abadi TS, Askari M, Miri K, Nia MN. (2020). Depression, stress and anxiety of nurses in COVID-19 pandemic in Nohe-Dey Hospital in Torbat-e-Heydariyeh city, Iran. Journal of Military Medicine. 22(6): 526-33. [Crossref] [Google Scholar] [Publisher]
- Helmy YA, Fawzy M, Elaswad A, Sobieh A, Kenney SP, Shehata AA. (2020). The COVID-19 pandemic: a comprehensive review of taxonomy, genetics, epidemiology, diagnosis, treatment, and control. Journal of clinical medicine. 9(4):1225. [Crossref] [Google Scholar] [Publisher]
- Malekpour-Dehkordi Z, Nourbakhsh M, Shahidi M, Sarraf N, Sharifi R. (2022). Silymarin diminishes oleic acid-induced lipid accumulation in HepG2 cells by modulating the expression of endoplasmic reticulum stress markers. Journal of Herbal Medicine. 33: 100565. [Crossref] [Google Scholar] [Publisher]
- Esmaeilzadeh AA, Yaseen MM, Khudaynazarov U, Al-Gazally ME, Opulencia MJ, Jalil AT. (2022). Recent advances on electrochemical and optical biosensing strategies for monitoring of microRNA-21: A review. Analytical Methods. [Crossref] [Google Scholar] [Publisher]
- Esmaeilzadeh AA, Kashian M, Salman HM, Alsaffar MF, Jaber MM, Soltani S, Amiri Manjili D, Ilhan A, Bahrami A, Kastelic JW. (2022). Identify Biomarkers and Design Effective Multi-Target Drugs in Ovarian Cancer: Hit Network-Target Sets Model Optimizing. Biology. 11(12):1851. [Crossref] [Google Scholar] [Publisher]
- Esmaeilzadeh A A, Rasoolzadegan S, Arabi A R, Soofi D, Rajaei Ramsheh S S, Saad Ahmed W, Moaref Pour R, (2022). Cytotoxic study of green synthesized pure and Ag-doped α-Fe2O3 nanoparticles on breast cancer (MCF-7) cell line Nanomedicine Research Journal 7 (4): 370-377. [Crossref], [Google Scholar], [Publisher]
- Rostami F, Tahernia H, Noorbakhsh M. (2022). Diagnosis and Treatment Of Guillain-Barre Syndrome And Neurological Problems With A Clinical Approach: A Systematic Review. Journal of Pharmaceutical Negative Results. 4094-111. [Google Scholar], [Publisher]


